Plantar Fasciitis
Plantar Fasciitis is caused by excessive strain on the Plantar Fascia. The plantar fascia is a band of tissue (fascia) which originates at the heel bone and extends to the insertion of all toes. The main function of the Plantar Fascia is to support the arch of your foot. Overtime if there is repeated strain over this fascia, tiny tears can occur and can lead to inflammation, pain and swelling. Plantar Fasciitis reportedly peaks in people between ages of 40 and 60 years in the general population and also in younger runners. Some younger active people can also suffer this condition such as those involved in running and dancing due to the nature of the movements.
You are more likely to suffer from Plantar Fasciitis if:
- Your feet roll in
- You walk, stand or run for long periods of time (especially on hard surfaces)
- You wear inappropriate or non-supportive footwear
- You are overweight
- You have tight achilles tendons and/or calf muscles
- You have low arched feet (increased strain on the heel bone will be exerted whilst walking).
- You have high arched feet (there may be increased strain on the heel area because the foot cannot roll in order to absorb shock)
- You have had a traumatic event resulting in excessive force through the arch of your foot
Clinical signs of Plantar Fasciitis include:
- Pain in the first steps in the morning
- Pain under the heel when weight-bearing
- Localised tenderness at the heel bone, or up along the arch
- Pain is gradual and dull
- Pain decreases as activity increases
- A history of other leg or foot problems
To help relieve pain & speed up recovery, please do the following list of treatments both morning and night!
Short Term
- Rest/reduce activity levels (especially running and jumping)
- In morning before getting out of bed:
- Write alphabet with your foot
- Make sure you step down onto shoes/sandles WITH arch support
- Wearing good supportive shoes most of the time
- Purchase new shoes (with good arch support) if old ones show excessive wear
- Icing – use a frozen coke bottle and roll under the arch of your foot, slowly increasing the force you use as you push down
- Stretching: BOTH LEGS STRETCH FOR 30 SECONDS (Right and Left)
- Gastrocnemius (calf muscle) – feet hip with apart with one leg in front of the other. Push against a wall keeping your back leg straight and heel on the ground. You should feel a stretch at the back part of your leg
- Soleus – feet hip width apart with one leg slightly in front of the other. Drop down with most of your weight going on the back leg. Should feel the stretch down the outside of the lower leg
- Self massage with voltaren gel or deep heat:
- First 3 minutes with big toe relaxed
- Next 3 minutes with toe dorsiflexed (pulled upwards)
- Strengthening exercises – picking up a tissue horizontally off the ground. Lift up your leg about 20cm off the ground and hold for 10 seconds. 3 sets of 10
- Low dye strapping – 1st day will feel tight, 2nd day will feel comfortable, 3rd day will start becoming loose. (podiatrist will show you how to do)
_____________________________________________________________________
- Anti-inflammatory medication; to reduce pain and inflammation (important to stop taking if causes stomach upsets. Contact GP if this occurs)
- Therapeutic Ultrasound
- Imaging; ultrasound, x-ray or bone scan
- Corticosteroid Injections
_____________________________________________________________________
Long term:
- Achieved with the use of customized orthotics (insoles that go inside your shoes) to help support the arch and reduce the plantar fascial movement
Heel Spur Syndrome/enthesopathy
Heel spur syndrome, enthesopathy, is defined as pain under the heel of the foot, due to the inflammation of the heel bone (calcareous) where it attached large ligament (plantar fascia). The spur growing out of the heel bone is actually bone calcification extending into plantar fascia. This condition often presents with plantar fasciitis.
Symptoms include: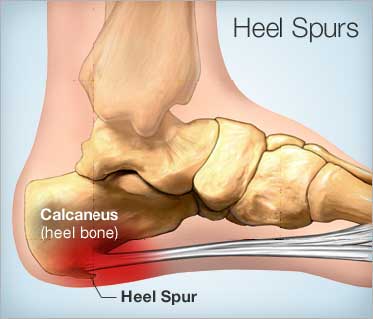
- Pain under the heel
- Pain worse following weight bearing activities
Risk Factors:
- Poor flexibility (eg. calf tightness)
- Poor biomechanics (eg. Over pronation)
- Inappropriate footwear
- Standing on hard surfaces
- overweight
Assessment – The podiatrists at toe-tal will diagnose the condition through a biomechanical assessment or X-ray, and go through all the necessary treatments listed below to help get you on the right path.
Treatment: – It is important to follow a rehabilitation program so your injury doesn’t reoccur.
- Rest/reduce activity levels (especially running and jumping)
- Ice for 15 minutes – use a frozen coke bottle and roll under the arch of your foot, slowly increasing the force you use as you push down
- Stretching and strengthening exercises – (talk to podiatrist what exercises require to do)
- Low dye strapping –(podiatrist at toe-tal will show you how to do)
- Take non-steroidal anti-inflammatory drugs (NSAIDs) for pain, maximum 7 days (contact GP if have any concerns)
- Orthotic therapy
- Correct biomechanics
- Wear good supportive shoes most of the time – (talk to the podiatrist at toe-tal about what footwear suits your foot best)
- Wear gel heel pad
- Lose weight if overweight
- Corticosteroid Injections
Contact Us.
Please contact the appropriate location for bookings.
Salisbury Medical Centre
PH: 3277 1621 - Fax: 3277 2887
ACE Sports Medicine – Hibiscus Sports Complex
PH: 3349 5733 - Fax: 3349 5122
Acacia Ridge Day And Night Chemmart Pharmacy
PH: 3277 4220 - Fax: 3255 5644
Brisbane Medical Specialists – Tarragindi
PH: 3184 0400 - Fax: 3892 7094
Morningside General Practice Clinics – Morningside Plaza
PH: 3399 4685 - Fax: 3395 7377
Any other enquiries please email info@toetalpodiatry.com.au or call 0422 389 652
